Q&A with Dr Michael Wagels: Tissue engineering

Q1. Tissue engineering is an unfamiliar concept to many people. Can you please explain what it is and how it is done?
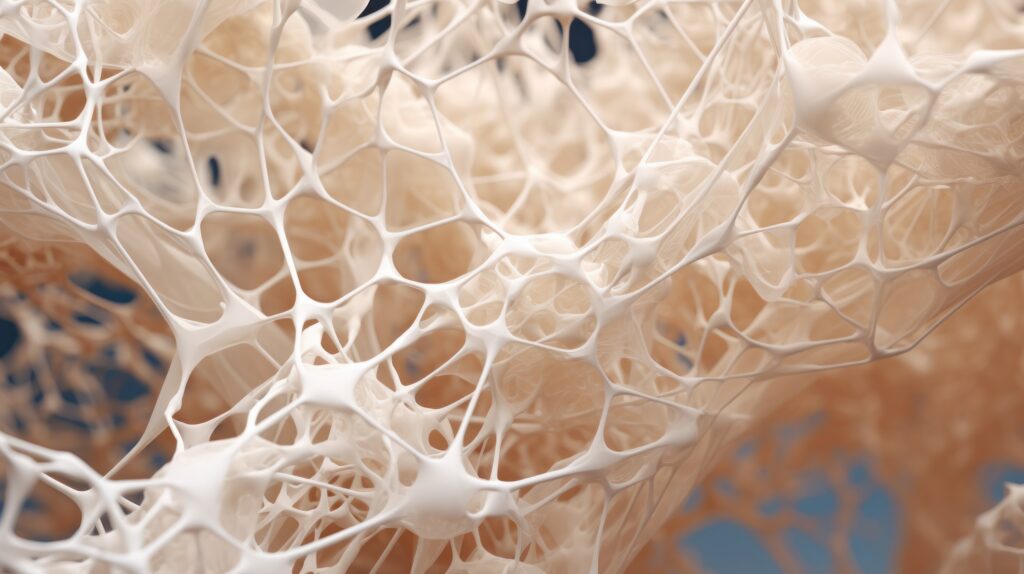
Tissue engineering is a discipline of biomedical engineering that endeavours to restore, maintain, improve or replace biological tissues. The key elements of any engineered tissue are cells, growth promoters and regulators, scaffold or matrix and a blood supply; summarised as the so-called “diamond concept”. It is driven by the same principles as plastic surgery but operates on a smaller scale. Bringing plastic surgery and bioengineers together will be very important in the near future, so that the successes achieved by bioengineers in the laboratory can be scaled up to solve complex reconstructive problems such as large bone defects, nerve injuries and large volume soft tissue defects.
Q2. I understand tissue engineering is a rapidly evolving area of research/surgery. Can you provide some history as to how this niche area developed and how it has changed over time?
Because the definition is a bit broad, a wide range of therapeutic approaches and devices have been referred to as tissue engineering. Some of this is marketing and some is misinformation but if we look at how tissue engineering evolved and look specifically for the diamond concept, it is easy to navigate.
Scientists have been trying to grow cells ex vivo since 1897. This culminated in Alexis Carrel more or less inventing cell culture, leading to him winning the Nobel Prize for medicine in 1912. Given the convergence of tissue engineering and plastic surgery mentioned earlier, it is fitting that he also features heavily in the history of microsurgery!
But culturing cells still isn’t tissue engineering per se. Materials science made some significant advances during the two World Wars, which informed progress in the development of implants but again, this can’t be considered tissue engineering. Stem cell research starting to become a legitimate science in the 1960s but it wasn’t until the 1970s that the key elements of tissue engineering were all brought together by Judah Folkman. He studied histogenesis in stem cells and worked out that proliferating cells needed a supportive matrix; morphogens such as growth factors and hormones, and vascularity. This is referred to as a bioreactor. Any development in the field since has sought to optimise one or several elements of this four-sided diamond concept.
Q3. Can you provide an update as to what successes, barriers/failures you have had, and what current clinical trials are underway?
My job has been to translate the successes of pre-clinical tissue engineering research into humans. This begins by getting directly involved in pre-clinical work, including animal studies, and making a concerted effort to understand the science. As a clinician, understanding the relevant aspects of cell biology was not difficult but I had to work hard to understand engineering principles. Exploring opportunities to use the human body as a bioreactor has been a very interesting exercise that involved blending together knowledge of axial vascular anatomy, rests of tissue with regenerative potential and donor site morbidity. Our greatest success was tissue engineering 36cm of missing tibia. The midface remains a challenge, being such a hostile and functionally demanding environment and we have learned an awful lot about the limitations of using the body as a bioreactor.
Clinical trials involving tissue engineering that are currently underway include the use of bioresorbable implants for large bone defects in load-bearing bone of the lower limb, membranous bone of the skull and mandible, camouflage correction of pectus excavatum deformity of the chest, volume replacement after removal of symptomatic breast implants and a 3D printed device for suture-less repair of nerve injuries. The last trial I mentioned is not so much tissue engineering but it is headed in that general direction.
Q4. How can it benefit patients, surgeons, and hospitals?
I think that the key benefit that tissue engineering offers is a robust solution to complex reconstructive challenges with fewer of the problems that we see in patients who survive their primary pathology. Patients are making it through their trauma or cancer treatment better than ever now, which means that they live longer with the consequences of tissue that is missing. If missing functional units could be replaced without the need for revision, without the risk of implant failure and without donor site morbidity, surviving might just be that little bit more worthwhile for patients and the health care system. I don’t see this doing reconstructive surgeons out of a job but it is important that we get intimately involved in turning great science into great clinical outcomes and cost savings in health care.
Q4. I gather there is huge potential for tissue engineering to be applied to the human body. What do you think the future holds for tissue engineering in surgery?
I see a time when it won’t be so necessary to use the body as a bioreactor. As I mentioned, I still see a role for plastic surgeons. For any given defect, the missing tissue can be replicated ex vivo; bringing small volume cellular elements from a patient into the laboratory, engineering the required tissue – or even an entire organ – to exact dimensions informed by clinical imaging, creation of a vascular network that is of sufficient size to be surgically manipulated, and then working out a way of returning it to the body from whence it came. I see potential in organoids, which are self-assembling groups of cells forming miniature functional organs, but more about that another time!
Featured Stories

ASPS welcomes new Ahpra guidelines for Non-Surgical Cosmetic Practitioners
Sydney. June 3, 2025: The Australian Society of Plastic Surgeons…
Continue reading Like
Like

