Information For Patients
Medicare funding confirmed for Abdominoplasty with muscle repair after pregnancy.
- Complaints Process
- Complications arising from surgery performed outside Australia
- Fees
- Is Your Surgeon an ASPS Member?
- Medicare funding confirmed for Abdominoplasty with muscle repair after pregnancy.
- Medicare funding confirmed for Abdominoplasty with muscle repair after pregnancy.
- Patient Updates
- Plastic Surgery Glossary
- Questions for Your Surgeon
- What Does FRACS Mean?
- What Does Specialist Plastic Surgeon Mean?
- What Training Does an ASPS Member Have?
- Will Medicare Cover my Procedure?
Medicare funding confirmed for Abdominoplasty with muscle repair after pregnancy.

Abdominoplasty Medicare Funding Confirmed
After reaching out to the community and to its Members in October 2021, The Australian Society of Plastic Surgeons (ASPS) campaigned to secure important support for their application to create a new Abdominoplasty Medicare item number for repair of rectus diastasis after pregnancy.
The addition of this procedure to the Medicare Benefits Schedule (MBS) is a welcome change that will have a positive impact on many women during a vulnerable period in their lives.
In response to recommendations from the Independent Medical Services Advisory Committee (MSAC), the Government has announced it will invest $6.6 million to reintroduce Abdominoplasty to the MBS as part of the 2022/23 budget.
This represents a major win for women who experience post-partum rectus diastasis.
The item number 30175 will be available on the MBS from the 1st of July 2022
Podcast
Trish Hammond from Plastic Surgery Hub interviews ASPS Vice President Dr Nicola Dean, and ASPS Community Advisor, Kerry Edwards regarding Abdominoplasty with Muscle Repair.
Listen to the podcast here
Frequently Asked Questions
Download our FAQ’s:
What do the recent announcements around surgical repair of rectus diastasis mean?
The Medical Services Advisory Committee (MSAC) advises the Minister for Health and the Commonwealth Department of Health on what procedures should be partially covered by Medicare (i.e. subsidised). Medicare used to cover surgery to sew the abdominal muscles back together after pregnancy, but it was removed from the Medicare Benefits Schedule (MBS) in 2016 due to concerns about its misuse for cosmetic purposes.
ASPS received the welcome news that their re-application or second application to MSAC, which was initially unsuccessful in 2018, had been supported.
The fact that MSAC has made a ruling to support an MBS item for the repair of rectus diastasis (tummy muscle split) for some women after pregnancy is a major win for those women.
Allocation for funds to support an item number for the procedure has been formally announced in 2022-23 Federal Budget.
The commencement date for the item number 30175 has been set for 1 July 2022.
Although the final item number has not yet been allocated, the criteria for assessing eligibility is listed below as per the PSD released by MSAC:
- Cause. The rectus diastasis (tummy muscle split) was caused by pregnancy
- Timing. The patient must be at least 12 months post-partum at the time of receiving the surgery
- Gap measurement. The gap between abdominal muscles must be at least 3cm as evidenced by diagnostic imaging.
- Symptoms. The patient must have documented symptoms of pain or discomfort at the site and/or low back pain or urinary symptoms
- Other treatment failed. The patient must have tried and failed to respond to non-surgical treatment options such as physiotherapy.
- Other examples of non-surgical treatment may be: symptomatic management with pain medication, lower back braces, lifestyle changes, physiotherapy and/or exercise.
To qualify for the procedure under Medicare, the decision ultimately sits with the Specialist Plastic Surgeon you see to determine whether you meet the criteria.
However, ASPS expect the following medical practitioners would have also been consulted with. ASPS would also expect those practitioners would provide the operating surgeon with confirmation of whether each patient may be eligible.
- GP would have been seen for non-surgical management and treatment options. GPs would also need to make the referral to the Specialist Plastic Surgeon who will perform the surgery.
- Physiotherapist or other Allied Health practitioner such as an Exercise Physiologist may be seen if the patient tried physiotherapy or exercise programs
- Radiologist must have conducted an ultrasound to measure and confirm the inter rectus diameter (the size of the gap between abdominal muscles)
Medicare is a Commonwealth Government scheme designed to provide rebates for treatment by registered health providers. It covers procedures that have been recognized as impacting people’s health, as well as consultations and other healthcare services. All Australian permanent residents and citizens have access to Medicare. However, for temporary residents or visitors, access to Medicare depends on your specific visa conditions.
If you do not have Medicare or Medicare rights, this recent announcement won’t change how you access this procedure and you will still need to pay full fees.
The factors listed below will impact how much you will pay.
- Medicare eligibility
- Private Health Insurance status and coverage
- Surgeon’s fee
- Final amount Medicare cover (this is called the ‘Schedule Fee’). The fee that has been allocated on the MBS schedule is $1025.60 with a benefit of 75% =$769.20 – this is an indication only.
- Hospital or surgical facility costs
- Anaesthesia fees
- Prescriptions for medication
- Post-surgery garments
- Medical tests, such as ultrasounds
- Any costs associated with non-surgical prior treatment, such as physiotherapy
Your surgeon should be able to discuss this in more detail with you.
For more information on Private Hospital, Public Hospital and Medicare costs please download the extended FAQ pdf document at the bottom of this page.
Medicare does not cover cosmetic procedures. A ‘tummy tuck’ is considered cosmetic. Those women seeking to improve the aesthetic appearance of their bodies rather than address a functional impairment will continue to have to pay the full cost of this procedure with no subsidy by Medicare or private health insurers.
This is why there are such tight eligibility criteria – to ensure it cannot be misused at the expense of public money.We urge patients and surgeons to ensure that the criteria for the procedure are clearly met before claiming this item, in order to prevent the misuse of Medicare funding. It is important to note that the procedure was removed from the Medicare Benefits Schedule (MBS) in 2016 due to concerns about its misuse for cosmetic purposes.
Medicare will also be conducting a review of usage of this procedure 2 years after it is implemented. If there is concern it is being misused for cosmetic purposes, we risk it being removed once again from the MBS to the detriment of those women who genuinely need this procedure for functional reasons.
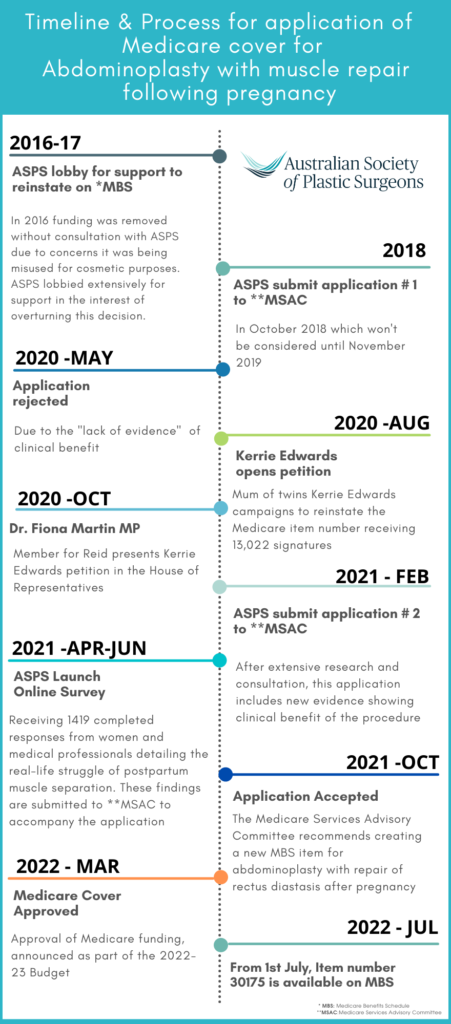
As is indicated in the Timeline below, this is a long and complex process. We can formally confirm that the item number will be available from the 1st of July 2022.
The number is set to come into effect from 1st of July 2022. There are a few things you can do in the meantime if you think you may be eligible.
- See your GP to discuss non-surgical treatment options or management of symptoms. These may include, but are not limited to: physiotherapy and/or exercise, symptomatic management with pain medication, lifestyle changes, lower back braces, etc. Bear in mind it will most likely be a requirement that you have tried to treat your rectus diastasis with non-surgical options before considering surgery. Your GP may refer you to a physiotherapist or other health professional to try non-surgical treatment options.
- Look into your Private Health Insurance options so any wait times for claiming certain procedures can be ticking over whilst awaiting this procedure to become available. See the above question – What does being covered by Medicare mean to me & what are the likely costs? For some information that might help you decide.
ASPS will be updating information as we receive it from the Department of Health on our webpage dedicated to this announcement and procedure. We suggest using ASPS information as we will receive direct updates from the Department of Health, which is responsible for overseeing MSAC’s support until implementation on Medicare.
To receive updates via email regarding the allocation of the new Medicare item number for abdominoplasty with repair of rectus diastasis after pregnancy, please complete the contact form provided below.
It would be helpful if you could indicate if you are a member of the public or a healthcare provider in the enquiry section below.
Given the tight eligibility criteria for this item number, ASPS expect there will be some women who may be experiencing some symptoms related to rectus diastasis but will not be eligible for this abdominoplasty under Medicare.
If you do not meet the Medicare eligibility criteria you can still have this procedure but will have to self-fund the full costs. Below are some other treatment or management options that may be applicable. As with any medical or health issue, this is just a list of some of the possible options and whether they are the right options for you will require a detailed discussion with your health care provider so your individual circumstances can be considered.
- GP management of symptoms
- Physiotherapy programs tailored to you and your symptoms (rectus diastasis, urinary incontinence, back pain etc.)
- Exercise programs aimed at improving core stability and functionality
- Sometimes rectus diastasis and hernias are related and there are some hernia procedures covered by Medicare so it might be worth discussing whether your symptoms could be managed through hernia repair with your GP.
- There are also currently existing item numbers for abdominoplasty but they are limited to patients who have experienced massive weight loss (not postpartum weight loss) and where there was an intraabdominal tumour that caused the rectus diastasis.
We understand that finding out about this news and discovering you may not be eligible can be hard to hear, so encourage you to talk with family, friends, and health care providers. Don’t forget you can also call Lifeline on 13 11 14.
This study will examine women with rectus diastasis undergoing abdominoplasty (tummy-tuck) and examine the health-related quality of life outcomes before and after the operation.
Who are we looking for?
- Australian women over the age of 18
- Women who have had at least 1 child who is 12 months or older.
- Women diagnosed with rectus diastasis, confirmed with abdominal ultrasound (inter-rectus distance is >30mm at any point along the linea alba).
- Women who have not had any previous abdominal surgery including weight loss surgery (Caesarean sections are ok).
- Women booked to undergo an abdominoplasty with muscle repair with an Australian Specialist Plastic Surgeon (FRACS(Plas)) who agrees to take part in the study.
- Women who have not undergone massive weight loss (>5 BMI point weight loss)
For more information on this study visit the AbdomiCARE website.
Timeline
The timeline indicates the journey starting from 2016 when the Medicare benefit was removed. In the 2022-23 Budget, funding was confirmed for this item number, and it came into effect on the 1st of July 2022.
Featured Stories

ASPS welcomes new Ahpra guidelines for Non-Surgical Cosmetic Practitioners
Sydney. June 3, 2025: The Australian Society of Plastic Surgeons…
Continue reading