Procedures
Breast Reconstruction
- About Your Specialist Plastic Surgeon
- Cosmetic
- Non-surgical Procedures
- Plastic Surgery Glossary
- Questions for Your Surgeon
- Reconstructive
- Surgical Procedures
- Abdominoplasty (Cosmetic)
- Abdominoplasty (muscle repair postpartum)
- Arm Lift
- Body Contouring
- Body Lift
- Breast Asymmetry Correction
- Breast Augmentation (Implants)
- Breast Implants with Lift
- Breast Lift
- Breast Reconstruction
- Breast Reduction
- Brow Lift
- Burns and Scarring
- Buttocks Lift
- Chest Surgery
- Chin Surgery
- Cleft Lip & Palate
- Ear Surgery
- Eyelid Reduction Surgery
- Facelift Surgery
- Facial Implants
- Facial Procedures
- Fat injection
- Genital Reconfiguration Surgery
- Gynaecomastia (Male Breast Reduction)
- Hair Replacement Surgery
- Hand Surgery
- Labiaplasty
- Liposuction
- Nipple Enhancement for Inverted Nipples
- Nose Surgery
- Scar Revision
- Skin Cancer
- Thigh Lift
- Tissue Expansion
- Voice Surgery
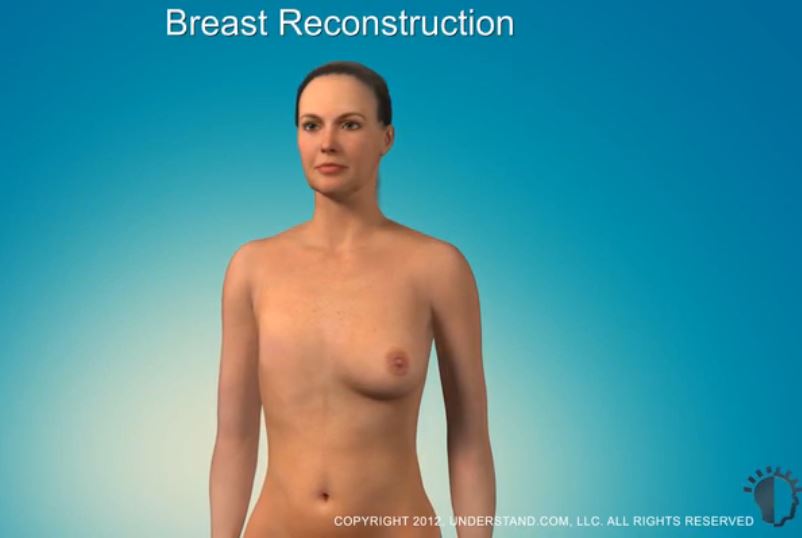
Breast Reconstruction
Any surgical or invasive procedure carries risks. Before proceeding, you should seek a second opinion from an appropriately qualified health practitioner.
Breast reconstruction is an increasingly common surgical procedure for women who have had a mastectomy. The procedure can create a breast that resembles a natural breast in appearance and form. Breast reconstruction is a physically and emotionally rewarding procedure for a woman who has lost a breast due to cancer or other condition.
Breast reconstruction is a surgical procedure that rebuilds a new breast or breasts to resemble a natural breast in appearance and form. Breast reconstruction is usually performed immediately after, or some time after a mastectomy.
There are two main types of breast reconstruction: implant reconstruction and flap reconstruction. In implant reconstruction, an implant is placed under the skin and muscle to recreate the shape of the breast. In flap reconstruction, skin, fat and muscle are taken from elsewhere on the body to make the new breast. The procedure best for you will depend on your age, general health, size and shape of the other breast, and available body tissue.
Breast reconstruction is a highly individualised procedure and may not be suitable for everyone. Always talk to your Specialist Plastic Surgeon before making a decision. Your Specialist Plastic Surgeon will assess your condition and general health, and plan the treatment that is best suited to you.
Before you decide on breast reconstruction surgery, there are some important issues to keep in mind:
- Breast reconstruction usually requires more than one operation
- Breast reconstruction with implants may not be a good option if you need to undergo radiotherapy as radiotherapy can cause the skin around the implant to shrink, This can cause scar tissue, may interfere with healing and could lead to leaking implants
Breast reconstruction may be a good option for you if:
- You are able to cope well with your diagnosis and treatment
- You do not have additional medical conditions or other illnesses that may impair healing
- You have a positive outlook and realistic goals for restoring your breast and body image
Remember that the procedure best for you will depend on your age, general health, size and shape of the other breast, and available body tissue. Discuss your options with your surgeon.
Breast reconstruction is performed under general anaesthesia. Modern anaesthesia is safe and effective, but does have some risks. Ask your Specialist Plastic Surgeon and anaesthetist for more information.
Your surgeon and/or anaesthetist will ask you about all the medications you are taking or have taken, and any allergies you may have. Make sure you have an up to date list before the surgery.
Modern surgery is generally safe but does have the potential for risks and complications to occur.
Some general complications and risks associated with surgery may include:
- Heavy bleeding from an operated site
- Fluid accumulation around the operation site(s)
- Infection that may require treatment with antibiotics or further surgery in some cases
- Allergic reaction to sutures, dressings or antiseptic solutions
- The formation of a large blood clot (haematoma) beneath an incision site may require further surgery
- Complications such as heart attack, pulmonary embolism or stroke may be caused by a blood clot, which can be life threatening
- Pain, bruising and swelling around the operated site(s)
- Slow healing, often related to smoking or diabetes
- Short-term nausea following general anaesthesia and other risks related to anaesthesia
Some possible complications and risks associated with breast reconstruction surgery using implants may include:
- Infection around the implant
- Capsular contracture, where firm scar tissue forms around the implant causing it to lose shape and softness
- Implant rupture or deflation
- Leakage of the implant’s contents (silicone gel or saline)
- Asymmetry (unevenness) of the breasts
- Calcium deposits in the scar capsule around the implant
- Granulomas, or lumps in local lymph node tissue formed by leaking silicone
- Movement of the implants from their original position
- Further surgery to treat complications
Some possible complications and risks associated with breast reconstruction surgery using flap reconstruction may include:
- Loss of blood circulation to the reconstructed breast due to clotting in the rejoined blood vessels. This can result in flap tissue dying (necrosis)
- Small areas of hardness (fat necrosis) may develop in the new breast
- Fluid collection (seroma) at the flap site
- Weakened abdominal muscle, which can result in a hernia
- Difference in size and shape (asymmetry) between the natural and reconstructed breasts
- Temporary loss of full movement of the arm on the side of the reconstructed breast.
Breast reconstruction surgery requires a short hospital stay of between two to five days, depending on your particular case.
You will also be asked to provide a complete medical history for your Specialist Plastic Surgeon including any health problems you have had, any medication you are taking or have taken, and any allergies you may have.
You may be advised to stop taking certain medicines such as non-steroidal anti-inflammatory drugs (NSAIDs), aspirin, and medicines that contain aspirin. You may also be asked to stop taking naturopathic substances such as garlic, ginkgo, ginseng and St John’s Wort as they may affect clotting and anaesthesia. Always tell your surgeon EVERYTHING you are taking.
You may be given medicines to take before the surgery, such as antibiotics.
Questions your surgeon may ask before the surgery include:
- Do you have an allergy or bad reaction to antibiotics, anaesthetic drugs or any other medicine?
- Do you have prolonged bleeding or excessive bruising when injured?
- Do you have a connective-tissue disorder such as rheumatoid arthritis, scleroderma, lupus erythematosis, or any other arthritis-like disorder?
- Do you have any long-term or recent illnesses?
- Have you previously had surgery for breast cancer, or radiotherapy to the breast?
- Have you had psychological or psychiatric illnesses?
Unless your surgeon advises differently, you will be able to continue taking most medicines that you have been taking.
Your surgeon will advise you if any other tests are required, such as blood tests, X-ray examinations or an Electrocardiograph (ECG) to assess your heart.
Prepare a “recovery area” in your home. This may include pillows, ice packs, a thermometer and a telephone within easy reach. Make sure you arrange for a relative or friend to drive you to and from the hospital or clinic. Someone should also stay with you for at least 24 hours after you return home.
Your surgeon should give detailed preoperative instructions. Follow them carefully.
After the surgery, your reconstructed breast may be covered with dressings. The nursing staff will change these regularly. With flap reconstruction, the new breast will, at first, be larger than the other breast. However, over the next few weeks, it will gradually become smaller to match your natural breast.
It is normal for your Specialist Plastic Surgeon to prescribe injections for pain relief. A plastic tube may be inserted into each breast to drain excess fluid. Other dressings may be changed or removed at this time.
Your surgeon will advise whether or not you should wear a bra immediately after surgery.
It is normal to feel tired and sore for the first two weeks. Avoid heavy lifting, strenuous exercise, swimming and strenuous sports until advised by your surgeon.
If you experience any of the following symptoms, notify your surgeon immediately:
- Temperature higher than 38°C or chills
- Nausea, vomiting, shortness of breath or diarrhea
- Heavy bleeding from the incisions
- Leakage of blood or fluid beyond the first day after surgery
- Worsening and/or spreading redness around the incision sites
- Increasing pain or tenderness in either breast
- Any other concerns or problems regarding your surgery, particularly if it appears to be worsening
Your surgeon will give you specific instructions on post-operative care. These instructions may include:
- How to care for your surgical site(s) following surgery
- Medications to apply or take orally to aid healing and reduce the risk of infection
- Specific concerns to look for at the surgical site(s) or in your general health
- When to follow-up with your surgeon
Be sure to ask your surgeon specific questions about what you can expect during your individual recovery period, such as:
- Where will I be taken after my surgery is complete?
- What medication will I be given or prescribed after surgery?
- Will I have dressings/bandages after surgery? If so, when will they be removed?
- Are stitches removed? When have they/will they be removed?
- When can I resume normal activity and exercise?
- When do I return for follow-up care?
Scars are an inevitable part of any invasive surgery. Your Specialist Plastic Surgeon will endeavour to minimise scarring and to keep your scars as inconspicuous as possible by locating the incisions in easily hidden sites. That way, scars will be along natural skin lines and creases. Scars may fade with time and become barely noticeable. If you are prone to scarring, you should advise your surgeon.
Breast reconstruction usually requires more than one operation to achieve the optimal outcome. Revisional surgery may also be necessary to correct minor irregularities.
Cost is always a consideration in elective surgery. Prices for individual procedures can vary widely between Specialist Plastic Surgeons. Some factors that may influence the cost include the surgeon’s experience, the type of procedure used and the geographic location of the office.
Costs associated with the procedure may include:
- Surgeon’s fee
- Hospital or surgical facility costs
- Anaesthesia fees
- Prescriptions for medication
- Post-surgery garments
- Medical tests
Your surgeon should welcome any questions you may have regarding fees.
- Areola:
Pigmented skin surrounding the nipple - Capsular contracture: A complication of breast implant surgery which occurs when scar tissue that normally forms around the implant tightens and squeezes the implant and becomes firm
- DIEP flap: Deep Inferior Epigastric Perforator flap which takes tissue from the abdomen
- Donor site: An area of your body where the surgeon harvests skin, muscle and fat to reconstruct your breast – commonly located in less exposed areas of the body such as the back, abdomen or buttocks
- Excision: To remove the skin
- Flap techniques: Surgical techniques used to reposition your own skin, muscle and fat to reconstruct or cover your breast
- General anaesthesia:
- Drugs and/or gases used during an operation to relieve pain and alter consciousness
- Grafting: A surgical technique to recreate your nipple and areola
- Haematoma: Blood pooling beneath the skin
- Intravenous sedation: Sedatives administered by injection into a vein to help you relax
- Latissimus Dorsi flap technique: A surgical technique that uses muscle, fat and skin tunnelled under the skin and tissue of a woman’s back to the reconstructed breast and remains attached to its donor site, leaving blood supply intact
- Local anaesthesia: A drug injected directly to the site of an incision during an operation to relieve pain
- Mammogram: An x-ray image of the breast
- Mastectomy: The removal of the whole breast, typically to rid the body of cancer
- Mastopexy: Surgery to lift the breasts
- SGAP flap: Superior Gluteal Artery perforator flap which takes tissue from the buttock
- Sutures: Stitches used by surgeons to hold skin and tissue together
- Tissue expansion: A surgical technique to stretch your own healthy tissue and create new skin to provide coverage for a breast implant
- TRAM flap:Also known as Transverse Rectus Abdominus Musculocutaneous flap, a surgical technique that uses muscle, fat and Transaxillary incision: An incision made in the underarm area
Visit the Plastic Surgery Glossary
for more medical terms.
This website is intended to provide you with general information only. This information is not a substitute for advice from your Specialist Plastic Surgeon and does not contain all the known facts about this procedure or every possible side effect of surgery. It is important that you speak to your surgeon before deciding to undergo surgery. If you are not sure about the benefits, risks and limitations of treatment, or anything else relating to your procedure, ask your surgeon to explain. Patient information provided as part of this website is evidence-based, and sourced from a range of reputable information providers including the American Society of Plastic Surgeons, Better Health Channel and Mi-tec medical publishing.
Featured Stories

AJOPS Blog: Exploring rural and regional issues
Providing plastic surgery services in rural and regional areas of…
Continue reading